
Leptospirosis in lion
Leptospirosis, caused by the Leptospira bacteria, is a zoonotic disease that poses a significant threat to both human and animal populations across the globe. While the disease is most commonly recognized in domestic animals such as dogs, cattle, and pigs, it also affects a wide range of wildlife species, including apex predators like lions (Panthera leo).
🐶 Pet Star
52 min read · 29, Mar 2025
Leptospirosis in Lions: Understanding the Impact of a Neglected Disease
Leptospirosis is a zoonotic disease caused by bacteria belonging to the genus Leptospira. This disease affects a wide range of animals, including both wild and domesticated species, and it can also be transmitted to humans. In wild animals, particularly large carnivores such as lions, leptospirosis is not always recognized or thoroughly understood, yet it poses a significant health threat. In this article, we will explore leptospirosis in lions, its epidemiology, clinical signs, diagnosis, treatment, prevention strategies, and the importance of raising awareness about this disease.
Introduction to Leptospirosis
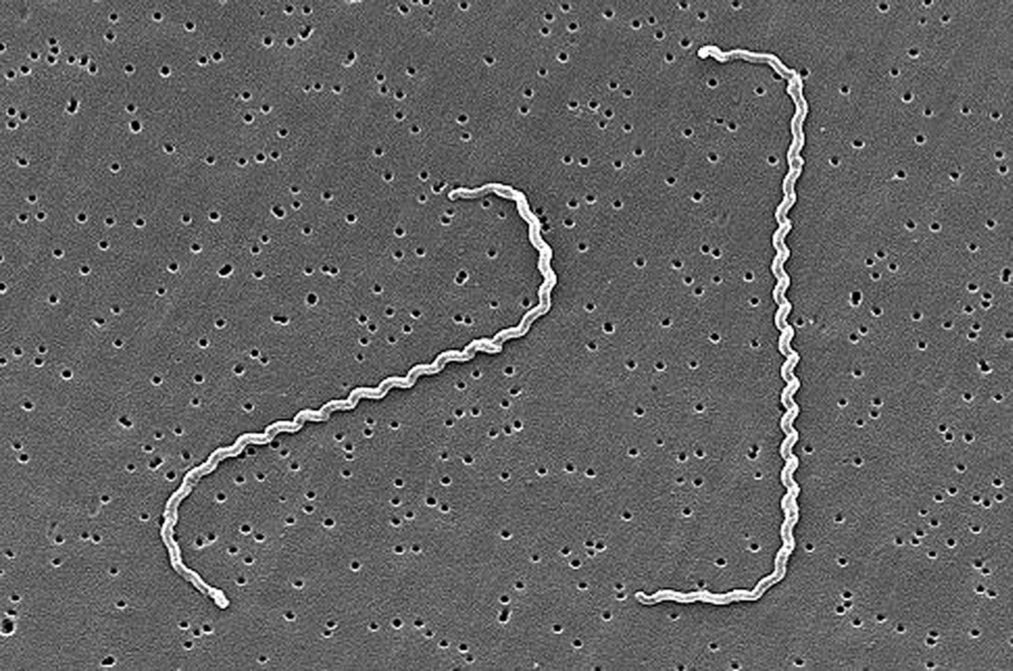
Leptospirosis is caused by a bacterial infection from the Leptospira species, which is typically found in the urine of infected animals. The disease is transmitted to other animals or humans through direct contact with urine or contaminated water, soil, or food. It is often associated with environments where water sources are contaminated, such as floods or poorly maintained enclosures.
Lions (Panthera leo), like other wild felines, have the potential to become infected with leptospirosis, but cases in these animals are less frequently reported compared to domestic species like dogs. However, understanding how leptospirosis affects lions is critical for wildlife conservation and veterinary care, as it can lead to severe health consequences, including kidney failure, liver damage, and even death.
Epidemiology of Leptospirosis in Lions
The primary route of transmission of leptospirosis in lions is through contact with contaminated water or soil. Lions, especially those living in wild habitats or protected reserves, are exposed to various wildlife species that act as reservoirs for Leptospira bacteria. These include rodents, cattle, and other carnivores, which may shed the bacteria in their urine. Lions can also acquire the infection indirectly through consumption of infected prey or through the environment.
The prevalence of leptospirosis in wild populations of lions is not fully understood due to limited surveillance and research. However, studies have shown that leptospirosis is more common in certain geographic areas, particularly where flooding and poor sanitation are prevalent. Lions in captive settings, such as zoos and wildlife reserves, may also be at risk if their enclosures are not properly maintained.
Clinical Signs of Leptospirosis in Lions
Leptospirosis presents in various ways, depending on the strain of bacteria, the immune system of the lion, and the severity of the infection. In lions, clinical signs can range from mild to severe, and in some cases, there may be no symptoms at all. The symptoms may develop gradually or appear suddenly, often following a period of exposure to contaminated water or food.
Common clinical signs of leptospirosis in lions include:
- Fever: One of the first signs of leptospirosis, fever is a common response to bacterial infections and is often present in the early stages of the disease.
- Lethargy and Weakness: Infected lions may exhibit signs of weakness, reluctance to move, or general lethargy.
- Loss of Appetite: Lions may become anorexic (refuse to eat), leading to weight loss and dehydration.
- Vomiting and Diarrhea: Gastrointestinal symptoms, such as vomiting and diarrhea, can occur in both acute and chronic cases of leptospirosis.
- Jaundice: Due to liver damage, lions with leptospirosis may exhibit yellowing of the skin and mucous membranes, a condition known as jaundice.
- Respiratory Distress: In severe cases, the infection may affect the lungs, causing respiratory distress or difficulty breathing.
- Kidney Dysfunction: One of the most severe manifestations of leptospirosis in lions is kidney failure. Infected lions may show signs of excessive thirst and urination, followed by a decrease in urine output.
Pathogenesis of Leptospirosis in Lions
Leptospirosis primarily affects the kidneys and liver in lions. Once the Leptospira bacteria enter the body, they travel through the bloodstream to various organs, including the kidneys, liver, and central nervous system. The bacteria multiply within these organs, causing inflammation and damage to the tissues.
The kidneys, in particular, are a common target for leptospirosis. The bacteria can damage the kidney tubules, leading to kidney failure. Infected lions may show signs of polyuria (excessive urination) followed by oliguria or anuria (reduced or absent urine production). Kidney failure can be fatal if not diagnosed and treated promptly.
Leptospirosis can also cause severe liver damage, leading to jaundice. The liver is essential for detoxifying the body, and when it becomes compromised, the lion may struggle to eliminate waste products from its body, leading to further complications.
In some cases, leptospirosis may also lead to the development of meningitis or encephalitis, inflammation of the brain and spinal cord. This can result in neurological signs such as seizures, paralysis, and altered behavior.
Diagnosis of Leptospirosis in Lions
Diagnosing leptospirosis in lions can be challenging because the clinical signs are often non-specific and can overlap with other diseases. Furthermore, wild animals like lions are not regularly tested for leptospirosis, meaning that many cases go undiagnosed or are misdiagnosed.
Veterinary professionals rely on several diagnostic methods to identify leptospirosis in lions:
- Serological Tests: Blood tests can detect antibodies against Leptospira bacteria. However, it is important to note that a positive result does not necessarily indicate an active infection, as antibodies can remain in the body long after the bacteria have been cleared.
- PCR (Polymerase Chain Reaction) Testing: PCR tests can detect the genetic material of Leptospira in the blood, urine, or tissues of the lion. This method is considered highly sensitive and specific for detecting active infections.
- Urine Testing: Since Leptospira bacteria are shed in the urine, testing urine samples for the presence of the bacteria is a key diagnostic tool.
- Histopathology: In some cases, tissue samples from affected organs (such as the kidneys or liver) may be examined under a microscope to identify characteristic signs of leptospirosis, including bacterial infiltration and tissue damage.
Treatment of Leptospirosis in Lions
Treatment of leptospirosis in lions typically involves the use of antibiotics and supportive care. Early diagnosis and prompt treatment are crucial for improving the chances of recovery and preventing complications.
- Antibiotics: Antibiotics such as doxycycline and penicillin are commonly used to treat leptospirosis in animals. These drugs target the Leptospira bacteria and help to eliminate the infection from the body.
- Fluid Therapy: Lions with leptospirosis may develop dehydration and electrolyte imbalances, particularly if they are vomiting or experiencing diarrhea. Fluid therapy is essential to maintain hydration and support kidney function.
- Liver and Kidney Support: In cases of severe liver or kidney damage, supportive treatments such as liver protectants, antioxidants, and medications to enhance kidney function may be necessary.
- Pain Management: Lions with leptospirosis may experience significant discomfort due to the fever, weakness, and organ dysfunction. Pain management is an essential aspect of treatment.
In severe cases, where organ failure has progressed, treatment may be less effective, and euthanasia may be considered to prevent unnecessary suffering.
Prevention and Control of Leptospirosis in Lions
Preventing leptospirosis in lions requires a multi-faceted approach that includes both environmental management and vaccination.
- Environmental Management: Ensuring that lion enclosures or habitats are well-maintained and free of contaminated water or waste is crucial. Regular cleaning of water sources and keeping the environment free of rodent infestations can significantly reduce the risk of transmission.
- Vaccination: Although there is no vaccine specifically for lions, some vaccines are available for domestic animals such as dogs. In some zoos or wildlife reserves, lions may be vaccinated with these vaccines as a preventive measure.
- Monitoring Wildlife Populations: In areas where wild lion populations are at risk, monitoring the health of both lions and potential reservoir species (such as rodents and cattle) can help detect outbreaks early and prevent further spread.
- Public Awareness: Raising awareness about leptospirosis among wildlife conservationists, veterinarians, and zoo staff is crucial for early detection and effective treatment.
Leptospirosis in Lions: A Critical and Understudied Health Threat
Leptospirosis, caused by the Leptospira bacteria, is a global zoonotic disease that poses a significant health risk to both humans and animals, including a wide variety of species such as dogs, livestock, and wildlife. Among these wildlife species, lions (Panthera leo), one of the apex predators in African and Asiatic ecosystems, are at risk for contracting leptospirosis, despite it being underreported in these populations. Although leptospirosis is more commonly studied in domesticated animals, such as dogs and cattle, its impact on wild species like lions remains relatively unexplored, with few documented cases in the wild. This bacterial infection is transmitted through contact with contaminated water, soil, or direct contact with urine from infected animals, which is particularly concerning in environments where lions live and hunt. Lions, particularly those living in the wild or in wildlife reserves, are exposed to an array of other animal species that serve as reservoirs for Leptospira, such as rodents, pigs, or even other carnivores. These animals shed the bacteria in their urine, and lions may become infected by drinking from contaminated water sources, consuming infected prey, or even coming into contact with infected urine from other animals in their environment. The bacteria enter the body through mucous membranes or broken skin and can rapidly spread through the bloodstream, eventually targeting vital organs, most notably the kidneys and liver. This can result in severe health conditions, including kidney failure, liver damage, jaundice, and, in some cases, meningitis or neurological complications. Lions infected with leptospirosis can display a variety of clinical signs, including fever, lethargy, loss of appetite, vomiting, diarrhea, and excessive thirst or urination. These symptoms may be subtle or indistinguishable from those caused by other diseases, making early diagnosis and treatment crucial for preventing irreversible damage or death. Furthermore, because leptospirosis in wild animals like lions is not routinely monitored, the true prevalence of the disease remains unclear, and many cases likely go undiagnosed or misdiagnosed, especially in the absence of specific surveillance programs. Diagnosis of leptospirosis in lions requires specialized tests, such as serology to detect antibodies, PCR (polymerase chain reaction) for bacterial DNA, and urine testing to identify the presence of the bacteria. These diagnostic methods, while effective, are not always readily available in the field, and in some cases, wild lions may go untreated due to the logistical challenges of wildlife veterinary care. If leptospirosis is diagnosed early, treatment involves the use of antibiotics, such as doxycycline or penicillin, which can effectively eliminate the bacteria from the lion's system. However, treatment is often complicated by the severity of the infection, as leptospirosis can rapidly progress to renal or hepatic failure, which requires additional supportive care like fluid therapy, electrolyte balance, and organ-specific treatments to stabilize the animal. If left untreated, leptospirosis can lead to long-term health complications or even death, making timely intervention critical. Prevention strategies for leptospirosis in lions are multifaceted and focus on minimizing exposure to Leptospira bacteria. In captivity, zoos, and wildlife reserves, controlling rodent populations, ensuring clean water supplies, and preventing the congregation of infected animals are essential steps in reducing the risk of infection. In addition, regular surveillance of wildlife populations in high-risk areas can help detect outbreaks early, allowing for prompt action to reduce the spread of the disease. While vaccines are available for domestic animals like dogs, no vaccine exists for lions or other large carnivores, and therefore, vaccination cannot be relied upon as a primary means of prevention. Instead, environmental management, along with careful monitoring of animal health, is crucial in preventing leptospirosis in lions. The risk of leptospirosis is particularly high in areas with heavy rainfall or flooding, which can cause contamination of water sources with Leptospira-carrying animal urine. This highlights the importance of maintaining dry, clean habitats and keeping enclosures or reserves free from waterlogged conditions. Additionally, raising awareness about leptospirosis among wildlife managers, veterinarians, and conservationists is essential for improving the detection and treatment of this disease, which remains a significant but underrecognized threat to lions' health. More research is needed to better understand the epidemiology of leptospirosis in wild felines, as well as the specific factors that contribute to the spread of the disease in different environments. By addressing these gaps in knowledge and focusing on preventative strategies, we can improve the health and conservation of lions and other wildlife species susceptible to leptospirosis. Ultimately, increasing our understanding of leptospirosis in lions will not only help in safeguarding the health of individual animals but also contribute to the broader goals of wildlife conservation, ensuring that populations of this iconic species continue to thrive in the wild while minimizing the risks posed by this potentially fatal disease.
Leptospirosis in Lions: A Hidden Threat to Wildlife Health
Leptospirosis, a bacterial infection caused by Leptospira species, is a major zoonotic disease that affects a wide variety of mammals, including both domestic animals and wildlife. While the disease is more commonly associated with species like cattle, dogs, and rodents, large carnivores such as lions (Panthera leo) are also vulnerable to this bacterial infection, albeit less frequently documented. In lions, leptospirosis is a neglected disease that is often overlooked, both in the wild and in captive populations. Understanding how leptospirosis affects lions is crucial for wildlife health, conservation efforts, and veterinary management in zoological settings. The disease is transmitted primarily through contact with water or soil contaminated by the urine of infected animals, with wild reservoirs being a significant source of bacteria. Lions, being apex predators in their ecosystems, may encounter Leptospira-infected prey, drink from contaminated water sources, or even become exposed to the bacteria via direct contact with urine from infected animals such as rodents, pigs, or cattle. This mode of transmission places lions in close proximity to the risk of infection, particularly in regions with poor sanitation, flooding, or densely populated wildlife environments. Once the bacteria enter the body through mucous membranes, broken skin, or ingestion, they target vital organs like the kidneys and liver, which are the primary sites of infection. Leptospirosis is capable of causing systemic damage, leading to conditions like liver failure, kidney dysfunction, jaundice, and in some cases, meningitis. This can result in severe symptoms, including fever, lethargy, loss of appetite, vomiting, diarrhea, and excessive thirst or urination, all of which are signs that veterinarians and wildlife managers must be vigilant about. The challenge of diagnosing leptospirosis in lions is exacerbated by the nonspecific nature of its clinical signs, which overlap with other common wildlife diseases. Furthermore, because lions are not routinely tested for leptospirosis in the wild, the true incidence of the disease in these populations remains poorly understood. Early diagnosis, however, can be achieved through the use of serological tests, PCR (polymerase chain reaction) for bacterial DNA, and urine testing, which are critical to identifying active infection and differentiating it from other diseases. Treatment typically involves antibiotics, such as doxycycline or penicillin, which are effective in eliminating Leptospira bacteria, as well as supportive care to address kidney or liver damage. Fluid therapy, liver protectants, and electrolyte management play a significant role in stabilizing affected lions. However, severe cases of leptospirosis may progress to organ failure, making early intervention essential for a favorable prognosis. Prevention of leptospirosis in lions can be achieved through a combination of environmental management and, in some cases, vaccination. In controlled environments like zoos and wildlife reserves, ensuring clean water sources, reducing rodent populations, and avoiding exposure to other infected animals are key preventive strategies. While vaccines for domestic animals exist, no specific vaccine is currently available for lions, and veterinary professionals often rely on general preventative measures, such as routine surveillance and early treatment. Conservation efforts that aim to preserve lion populations in the wild must include strategies for monitoring disease outbreaks, particularly in areas prone to flooding or other environmental factors that increase the risk of leptospirosis transmission. Ultimately, greater awareness and research into leptospirosis in wild felines will be essential in ensuring that lions and other wildlife species are adequately protected from this potentially fatal disease, safeguarding their health and ensuring the sustainability of their populations in both captivity and the wild.
Conclusion
Leptospirosis is a serious, often underdiagnosed disease that can have significant health consequences for lions. While research on leptospirosis in wild felines is limited, it is clear that lions are vulnerable to this bacterial infection, particularly when they live in environments where contamination is prevalent. Timely diagnosis, appropriate treatment, and preventive measures such as environmental control and vaccination are critical for protecting lions from this disease.
As we continue to study leptospirosis in wild animals, it is essential to improve surveillance and awareness to mitigate the risks associated with this neglected disease. By taking proactive steps, we can help ensure that lions and other wildlife species are better protected from the impacts of leptospirosis and other emerging zoonotic diseases.
Summary
Leptospirosis is a bacterial infection that poses a significant health risk to lions, particularly in environments where contamination with Leptospira bacteria is prevalent. The disease primarily affects the kidneys and liver, leading to severe symptoms such as fever, lethargy, vomiting, jaundice, and kidney failure. Diagnosing leptospirosis in lions can be challenging,
Q&A Section: Leptospirosis in Lions
Q1: What is leptospirosis and how is it transmitted to lions?
Ans: Leptospirosis is a bacterial infection caused by the Leptospira bacteria. It is transmitted to lions primarily through contact with water, soil, or surfaces contaminated with the urine of infected animals. Lions can become infected by drinking contaminated water, consuming infected prey, or coming into contact with infected urine from animals such as rodents, livestock, or other wildlife.
Q2: What are the symptoms of leptospirosis in lions?
Ans: The symptoms of leptospirosis in lions can vary but commonly include fever, lethargy, loss of appetite, vomiting, diarrhea, excessive thirst, and frequent urination. As the infection progresses, lions may experience jaundice (yellowing of the skin and mucous membranes), kidney failure, and in severe cases, liver damage and neurological complications.
Q3: How is leptospirosis diagnosed in lions?
Ans: Leptospirosis in lions is diagnosed using specialized tests such as blood serology, PCR (polymerase chain reaction) testing for bacterial DNA, and urine analysis. These tests help identify the presence of Leptospira bacteria or antibodies against the bacteria, confirming an active infection. Early diagnosis is critical for effective treatment.
Q4: What is the treatment for leptospirosis in lions?
Ans: Treatment for leptospirosis in lions typically involves the use of antibiotics such as doxycycline or penicillin, which are effective in eliminating the Leptospira bacteria. Supportive care is also important, including fluid therapy to help maintain hydration and kidney function, as well as pain management. In severe cases, additional treatments may be required to address complications like kidney or liver failure.
Q5: Can leptospirosis be prevented in lions?
Ans: Prevention of leptospirosis in lions focuses on reducing their exposure to contaminated environments. In captivity, this involves controlling rodent populations, ensuring clean water sources, and maintaining proper hygiene. In the wild, monitoring water quality and reducing exposure to infected prey or other animals are important preventive measures. However, there is no vaccine currently available for lions, so environmental management is key.
Similar Articles
Find more relatable content in similar Articles
Explore Other Categories
© 2024 Copyrights by rPets. All Rights Reserved.